Dr. Craig Smith says he once held the same misconceptions that many doctors have about bringing Suboxone – which is used to treat opioid addictions – into his practice.
Difficult patients. An overwhelming demand. A constant headache. Endless red tape.
“I thought it would be a big disruption. I thought I would have a lot of people looking like Keith Richards on my doorstep,” said Smith, referring to the Rolling Stones guitarist who has battled substance abuse.
Instead, Smith said that since he started prescribing Suboxone seven years ago, he’s helped numerous people improve their lives, and the patients have not been disruptive to the practice.
“It’s turned out to be the most gratifying part of the job,” said Smith, of Bridgton. “People come to you and they have hit rock bottom, and you’re helping them get back on their feet. Some of them, within weeks, they’re back in your office, smiling, and they’ve started to put their lives back together.”
The Maine Medical Association, an advocacy group representing physicians before the Legislature, is working hard to persuade more doctors to prescribe Suboxone to combat the state’s growing heroin crisis, because there’s a wide gulf between the supply and the demand for treatment.
Doctors must first undergo eight hours of training before being permitted to treat up to 100 patients with Suboxone, a pill that reduces cravings for opioids. Between 25,000 and 30,000 Mainers want drug treatment but don’t have access, according to the U.S. Substance Abuse and Mental Health Services Administration.
Lisa Letourneau, executive director of Maine Quality Counts, a health advocacy group, said Maine needs many more of its doctors to become Suboxone providers.
“Until we can get Suboxone into primary care practices, we will never have enough capacity in Maine,” Letourneau said.
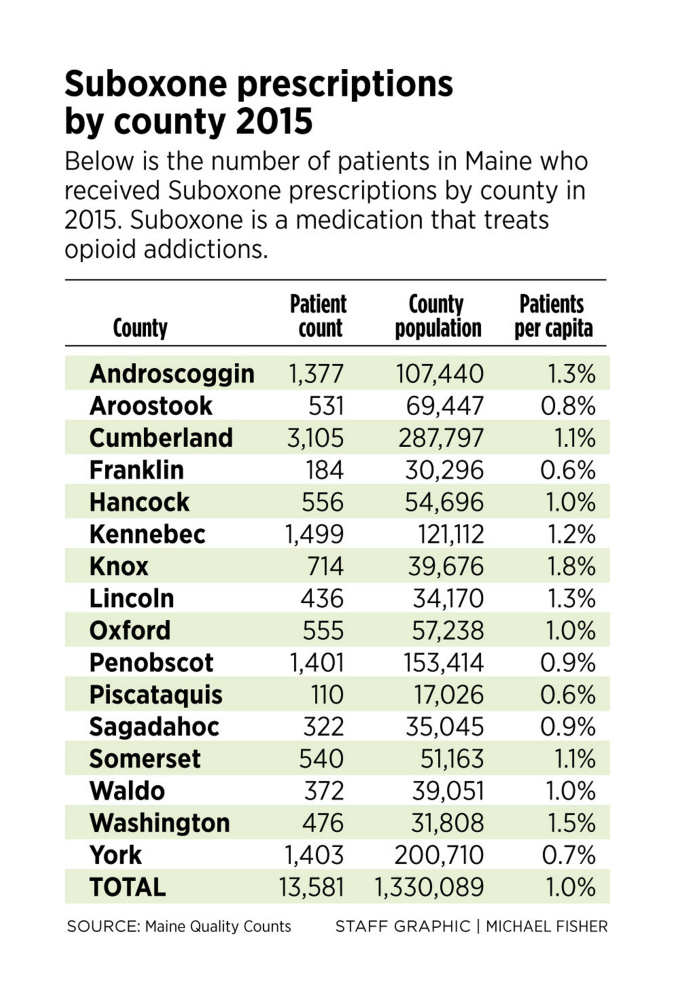
There are 214 doctors, including primary care physicians and addiction specialists, actively prescribing Suboxone out of the roughly 2,000 primary care doctors in the state, according to figures provided by the medical association and Maine Quality Counts. About 13,500 Maine patients received a Suboxone prescription in 2015.
The shortage of prescribers is not just a Maine problem. Access to medication-assisted treatment is lacking across the United States, according to a study published last week in the Journal of the American Medical Association. The study estimated that only 2.2 percent of all doctors in the U.S. have completed Suboxone training, and that half of all opioid addicts have no access to medication-assisted treatment.
So far, persuading doctors to become Suboxone providers is slow going, and the need is daunting, officials say.
Maine has thousands of people addicted to opioids and not nearly enough doctors able to treat them effectively.
“We have a lot of work ahead of us,” said Gordon Smith, the medical association’s executive director. Smith said he believes minds are being changed, but it’s difficult to know whether it will translate into more doctors becoming Suboxone prescribers.
“There’s some reluctance from physicians to get involved in this,” he said.
FIXING MESS CREATED BY DOCTORS
Smith said that between now and the end of the year, he will be traveling the state and hosting 50 events for doctors, in part to try to persuade them to bring Suboxone into their practice. Maine had a record 272 drug overdose deaths in 2015, with most caused by opioids.
Suboxone can be picked up at a pharmacy, unlike methadone, which is usually dispensed in cups at standalone clinics. Methadone is typically recommended for the most severe opioid addictions, but Suboxone can be prescribed for many patients.
Dr. Elisabeth Fowlie Mock, a primary care physician from Holden, said doctors, along with the pharmaceutical industry, created the opioid crisis by overprescribing opioids for pain relief, starting in the late 1990s and early 2000s. Four out of five heroin addicts were first addicted to prescription opioids, according to the American Society of Addiction Medicine.
“We have to own the fact that we created this tremendous mess,” said Mock, who will receive Suboxone training next month. “And now we have to be the ones to fix it.”
The medical association and Maine Quality Counts hosted a conference July 14 that discussed the dangers of prescribing opioids and how to comply with a new law that places a dosage cap on them, and also included discussions on Suboxone.
“We’re at the very beginning of addressing this problem,” said Eric Haram, who heads up a medication-assisted treatment program through Mid Coast Hospital in Brunswick that’s being recognized as a model for access. But the Brunswick program is the exception.
The federal government is also working to expand treatment by increasing the cap on Suboxone patients per physician from 100 to 275. And Congress passed a law that will give nurse practitioners and physician assistants the authority to prescribe Suboxone, after completing training.
“That will be a great help,” said Smith, estimating that there are about 1,300 nurse practitioners and 700 physician assistants in Maine.
Increasing the cap to 275 patients would also be helpful, Smith said, but it doesn’t change the fact that there needs to be more doctors willing to prescribe Suboxone.
The federal government places a cap on the total number of patients each doctor can prescribe to discourage unscrupulous doctors from becoming “pill mills.”
BOTH MOMENTUM AND RESISTANCE
The Maine Opioid Collaborative, a group consisting of people in the treatment community, public health system, hospitals, law enforcement, former addicts and others, concluded in May that expanding access to medication-assisted treatment would be the most effective way of dealing with the opioid crisis.
The collaborative pointed to research that shows how medication-assisted treatment is scientifically proven to work, while abstinence-based programs have a much higher relapse rate.
U.S. Sen. Angus King, a Maine independent, said there seems to be momentum on providing greater access to medication-assisted treatment.
“I’ve seen a change in the last two to three years regarding people’s attitudes on the subject. We have to expand access, as the problem we have with opioids is staggering,” King said.
Dr. Smith, the Bridgton physician, said that for doctors, it’s “really hard to make that first step” to become a Suboxone provider.
“Doctors don’t like to do things that are uncharted territory for them,” he said.
For Smith, what he saw in his practice spurred him into becoming a Suboxone provider.
In August 2009, four of his patients died from opioid-related drug overdoses. Alarmed, Smith did Suboxone training and soon thereafter began accepting patients.
“It opened my eyes and made me realize the problem is much bigger than we thought,” Smith said. He said his patients were using opioids but hiding it from him, so every time the medical examiner called, he was surprised to hear that toxicology tests revealed the presence of opioids. “It made me realize this is something we should be doing,” he said.
Smith’s wife, Dr. Jennifer Smith, is also a Suboxone provider and works in the same office, so they treat about 200 opioid patients at the same time.
He said about 60 percent to 70 percent of Suboxone patients need to remain on a low maintenance dose of Suboxone.
The practice can accept all patients, even the uninsured, Smith said. They work closely with Crooked River Counseling so that Suboxone patients can be paired with a therapist.
Smith said that after he started seeing positive experiences with Suboxone, he began telling other doctors about it, and now there are six doctors in the region – soon to be seven – who prescribe Suboxone.
BARRIERS TO MORE PRESCRIBING
Letourneau, of Maine Quality Counts, said there are many barriers to persuading doctors to prescribe Suboxone, and one is institutional resistance. She said many of the state’s hospitals have either not yet bought into the concept or are slow to do so, in part because of society’s “overwhelming bias and stigma” against drug addicts.
“In many cases, it’s not the doctor’s individual decision. Our institutions haven’t yet addressed this crisis in a systemic way,” Letourneau said. “There has not yet been an organizational commitment to take this on.”
Most primary care doctors in Maine are connected to a hospital network, such as MaineHealth or Eastern Maine Healthcare Systems.
Letourneau said some doctors may also feel held back from taking on Suboxone patients by bureaucratic requirements, which stifle their desire to treat patients with addictions.
Haram said Maine’se government could do a better job of recruiting Suboxone providers, going after grant money for training, and connecting Suboxone providers with counseling services.
“Doctors who choose to do this want to be supported,” Haram said “They don’t want to hang their shingle out for their 100 Suboxone patients and not have any counseling support.”
Haram said that despite the difficult task ahead, people are at least talking about and focused on the issue, so perhaps significant changes are ahead.
Letourneau agreed, and said that even though Maine has only a “tiny fraction” of the doctors needed to prescribe Suboxone, at least people seem more open-minded lately about treating addiction.
“There’s a buzz, a conversation about this topic that we weren’t having a few years ago,” she said.
_________________________________
CORRECTION: This story was updated at 5:24 p.m. on Dec. 30, 2016, to clarify that doctors prescribing Suboxone include primary care physicians and addiction specialists.
Send questions/comments to the editors.