Maine hospitals have doubled the amount of free care they provide over the past five years as the weak economy pushed more people out of work and companies shifted an increasing amount of health care costs onto employees.
“The economy is having a significant impact,” said Sue Hadiaris, vice president of planning and development at Southern Maine Medical Center in Biddeford. “As the economy continues to stay stagnant, companies are changing insurance. People are adjusting what insurance they carry, and other people have lost insurance.”
More scrutiny has been placed on free care as health care has become big business and top hospital executives in Maine fetch six-figure salaries. Hospitals vary in the types and amounts of free services they provide, as well as how they disseminate charity care information to their patients, advocates said.
As more people apply for free care, hospitals must balance the legal requirement to provide charity services to the poor with the need to be prudent about collecting bills and investing in facility improvements in order to remain competitive.
Mercy Health System recently hired Accretive Health, which was sued in January by the Minnesota Attorney General’s Office amid claims it violated patient-privacy and debt collection laws by posting bill collectors in emergency rooms and at patient bedsides. Mercy has said no aggressive bill-collection tactics would be tolerated at its hospital, and noted that it provided more charity care than area hospitals.
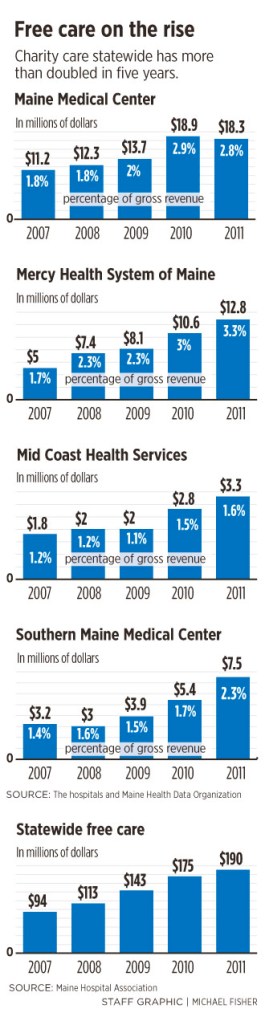
A Portland Press Herald survey of the four largest hospitals in the Greater Portland area found that Mercy Health System provides more free care as a percentage of its gross revenues than its peers. Mercy, a Catholic hospital, last year spent about $12.8 million — 3.3 percent of its gross revenues — on providing free care. Its charity care costs have more than doubled in the past five years, and applications for free care have risen each month, said Chief Financial Officer Tony Marple.
“It’s kind of hard to predict. We don’t try to control the number of charity cases,” Marple said. “It has a negative impact on profitability. … It’s a challenge.”
Nancy Berlinger, a research scholar at The Hastings Center, an independent, nonprofit bioethics research institute in Garrison, N.Y., said hospitals have to clearly distinguish between the free care they must provide and the bad debts or bills they can’t collect.
“Hospitals have to do their best to recoup fees they are legitimately owed,” said John Gale, a research associate focused on hospitals, charity care and community benefits at the Muskie School of Public Service at the University of Southern Maine. “The question is how and when hospitals make it clear that charity care is available.”
BAD DEBTS RISE WITH CHARITY CARE
Maine’s 36 nonprofit hospitals are required by the state to provide medically necessary free care to patients with incomes at or below 150 percent of federal policy guidelines. For a family of four, the income level is $2,882 a month, or $34,584 a year, to qualify for free care, according to Consumers for Affordable Health Care.
Maine’s median household income was $46,933 from 2006 to 2010, according to the U.S. Census Bureau.
“It’s always been a challenge to manage charity care. We saw a real spike in 2009 and it’s been going from there,” said Mid Coast Hospital Chief Financial Officer Robert McCue. “It’s very challenging. It’s become a new cost just like any other cost. You do your best not to pass that cost on, but at some point it becomes so large that taxpayers and insurance companies end up paying for it.”
Statewide, charity care totaled $190 million in 2011, double the amount offered five years ago, according to the Maine Hospital Association. Bad debts, or uncollected bills, at hospitals rose to $209 million, up 34 percent from 2007, the association said.
Since nonprofit hospitals are exempt from state, local and federal taxes, some health care advocates argue that the institutions should be more liberal with their free care policies.
“There are concerns that hospitals have not provided as much community benefit as they get through their tax-exempt status,” said Alwyn Cassil, director of public affairs for the Center for Studying Health System Change in Washington. “A lot of it comes down to hospital missions and boards of trustees, who are members of the community, who are guiding the hospitals and meeting or not meeting community needs.”
HOSPITALS TRY TO CONTROL COSTS
While there is no direct link between tax exemptions and charity care, some advocates use taxes as the benchmark for what the hospitals save and what they could be shifting toward free care. Twelve of Maine’s hospitals received more than twice as much money in local property tax breaks — $116.8 million — than all of the state hospitals combined gave in charity care in 2005 ($60.6 million), according to Consumers for Affordable Health Care. That was the most recent year for which data was available.
The Patient Protection and Affordable Care Act requires hospitals to assess community health care needs and inform patients of their charity care policies. The fact that a needs assessment was mandated “reflects concerns on the part of policymakers that hospitals have not embraced this charity care requirement as closely as they should,” Cassil said.
Each hospital has responded differently to the surge in demand for free care.
For example, Mid Coast Hospital in Brunswick, which has seen an 80 percent increase in free care over the past five years, has opened a clinic to connect patients with MaineCare, the state’s Medicaid program, which receives about two-thirds of its funding from the federal government. The clinic helps link patients to subsidized or free care and keeps them from using the costly emergency room as their main source of medical care.
Meanwhile, Southern Maine Medical has bought PrimeCare Physicians, which put primary care and specialists under the umbrella of its nonprofit hospital. That means those doctors’ services can be provided for free to poor patients. Southern Maine also has an employee who meets with patients to see if they qualify for federal aide, free care or insurance programs.
FREE CARE LESS OF A PATIENT STIGMA
One 55-year-old Falmouth woman said she has been receiving free care for 30 years at the Adult Internal Medicine Clinic at Maine Medical Center. The woman, who legally changed her name to just “Terry,” said the clinic has improved its care and customer service over the years that she has been a patient.
“It’s much, much easier now. I used to feel like the scum of the earth. Now they make you feel good. The demeanor has changed. The world has changed. People are realizing that there’s people who need care and that doesn’t make them bad,” said Terry, who teaches violin.
Terry has gone through costly procedures, such as childbirth and hip replacement, with only a $10 co-pay.
There’s no minimum national requirement for the amount of free care that hospitals offer. The American Hospital Association said hospitals provide $39.3 billion in uncompensated care — but that includes both free care and bad debts, or bills that patients don’t pay. The association said the total of uncompensated care as a percentage of expenses was 5.8 percent.
In the past, Washington lawmakers have discussed setting national rules that nonprofit hospitals must provide charity care equal to 5 percent of their revenues. States such as Texas and Pennsylvania already require just that, in order for hospitals to keep their nonprofit tax breaks. Illinois also is considering such requirements, Gale said.
But having a minimum requirement may not be the answer, health care advocates said.
“One caution to having a federal requirement is that it could become a ceiling for what hospitals provide, not a minimum. The needs in each community are different, so a standard requirement may not work,” said Jessica Curtis, hospital accountability project director for Community Catalyst in Boston, a national advocacy group.
Many patients don’t even know they qualify for free care or don’t know the hoops to jump through to get it.
A 2009 survey of 99 hospitals nationwide by Community Catalyst and The Access Project, another Boston-based health advocacy group, found that 85 percent of hospitals mentioned charity care to patients. But compliance dropped off to fewer than half when it came to providing applications for financial help, and only one-quarter provided eligibility requirements on their websites.
“Not-for-profits get pretty significant tax write-offs for providing free care, and still, it’s not uncommon for us to hear about hospitals not posting policies, aggressive collection tactics or inconsistent policy implementation,” Curtis said.
Staff Writer Jessica Hall can be contacted at 791-6316 or at:
jhall@mainetoday.com
Send questions/comments to the editors.